Professor Hui-Ching Lin (left), Dr. Cheng-Ta Li (middle) and postdoctoral research fellow, Chi-Wei Lee (right).
Despite the availability of medication for treating depression, some patients still struggle to improve effectively. A recent animal experiment has revealed a potential solution for treatment-resistant depression through brain magnetic stimulation techniques. This non-invasive therapeutic approach enhances synaptic plasticity in the brain, thereby offering more compelling scientific evidence.
Repetitive transcranial magnetic stimulation (rTMS) is a clinically established treatment method involving the placement of a coil on the scalp to activate brain neurons using electromagnetic waves. For patients who have not responded significantly to the use of two or more antidepressant medications, rTMS offers new hope. While its efficacy is evident, the underlying mechanism of action remains elusive.
Researchers, led by Professor Hui-Ching Lin from our college’s Institute of Physiology, in collaboration with Dr. Cheng-Ta Li, Chief of the Division of Community and Rehabilitation Psychiatry at Taipei Veterans General Hospital, have successfully established a rat model of depression. This study confirms that either intermittent theta burst stimulation (iTBS) or continuous theta burst stimulation (cTBS) can improve pro-brain-derived neurotrophic factor (proBDNF) in the prefrontal cortex. Additionally, the decline in brain-derived neurotrophic factor BDNF can be reversed using iTBS.
This groundbreaking research provides scientific validation for the application of two distinct magnetic stimulation methods in the molecular biological mechanisms underlying the treatment of depression.
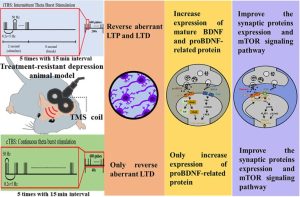
To establish scientific evidence, the research team subjected rats to electric shocks on their paws, mimicking a traumatic situation. Following intensive electric shocks, the team observed depression-like behaviors in rats through sucrose preference, forced swim test, and tail suspension tests, and which did not response to typical antidepressant, including fluoxetine, imipramine and venlafaxine, thus creating the treatment-resistant depression. After transcranial magnetic stimulation, the depression rats exhibited significant therapeutic effects on depressive and active coping behaviors, as evident from both electrophysiological signals and molecular biochemical analyses.
Leading the study, Professor Hui-Ching Lin emphasized that around thirty percent of depression patients remain unresponsive to active treatment efforts. In 2018, Taiwan’s Food and Drug Administration approved the use of rTMS for treating depression patients with inadequate responses to medication. Professor Cheng-Ta Li, designer of this study, also highlighted collaborative efforts between Taipei Veterans General Hospital and National Yang Ming Chiao Tung University in conducting large-scale controlled studies that confirmed the antidepressant effects of iTBS on the prefrontal cortex. This research contributes to bolstering clinical treatment with stronger scientific support.
Chi-Wei Lee, a postdoctoral researcher involved in the study, also noted that low-dose ketamine injections have been considered an option for treatment-resistant depression. This animal experiment further revealed that rTMS regulates the drug pathway.
The current challenges in treating depression encompass cases of lack of treatment and ineffective medication. This animal model study has been published in Journal 《Experimental Neurology》. This research acknowledges the contributions of NYCU Brain Research Center and Dr. Nai-Kuei Huang of the National Research Institute of Chinese Medicine for their assistance in animal experiment.
Source: https://www.nycu.edu.tw/news/4924/